Many of the deaths of children who died from sepsis in recent years could have been avoided, a
new report published today has found.
The National Child Mortality Database at the University of Bristol has found that over the 3 years to March 2022, around 15% of deaths in children were linked to infections. Almost half of those had sepsis. In actual fact, the proportion is likely to be higher, because sepsis is often missed or not recorded properly.
In 18% of the deaths caused by sepsis, the report found there were contributory issues suggesting the clinicians hadn’t recognised sepsis or acted quickly enough. Issues included delays in recognising the child’s condition was deteriorating, in arranging senior reviews of the child, and/or in providing appropriate treatment for sepsis. Another issue identified was that parents’ concerns about their child’s condition were not always listened to.
This means that opportunities were missed to diagnose and treat sepsis earlier in more than 150 children, opportunities which had the potential to save lives.
The report follows the news in October that the ombudsman for health services in the UK had found there had been little improvement in the figures for diagnosing and treating sepsis over the past 10 years, and that too many people are still dying from sepsis due to the same mistakes being made.
There is clearly still more work to be done to ensure clinicians follow the sepsis guidelines for diagnosis and treatment, and that they listen to parents’ concerns about their children.
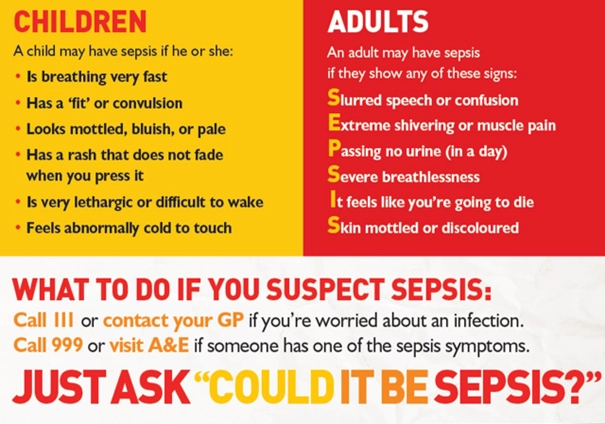
What is sepsis?
Sepsis is a life-threatening reaction to an infection. It happens when your body overreacts to an infection and starts attacking its own tissues and organs. It is not a rare condition; it affects 245,000 people a year in the UK alone, 48,000 of whom will die. That is more than breast, bowel and prostate cancer combined. 2,000 children a year die from sepsis. It is very important to know the signs.
It can happen to anybody, but some people are more at risk than others, including people who have recently had surgery, people with lowered immune systems, elderly people and children, particularly babies under 1.
William Mead
William Mead was a one-year-old little boy who had had a lingering cough for weeks. On 12 December 2014, he became more unwell, crying and uncomfortable, very tired, not eating and with a high temperature.
His mother sought help from the family’s GPs, NHS 111 and their local hospital over the following day and a half. Each time, she told them about William’s worsening condition – he had become very pale, was cool to the touch, he had stopped having wet nappies, was refusing anything to drink and kept vomiting. They all dismissed it as a viral infection, and his parents were told not to take William to A&E because his condition wasn’t urgent.
On the morning of 14 December 2014, less than two days after William had become very unwell, his mother went into his room to check on him and found that he had died in the night.
William’s lingering cough had been caused by the bacteria Group A Streptococcus (Strep A), which had developed into sepsis. An investigation by NHS England found that there had been 16 failings in care, and 4 missed opportunities to save William’s life.
William should be 10 years old now. Since he died, his mother, Melissa Mead, has become one of the foremost campaigners for improving awareness of sepsis. She has worked with UK Sepsis Trust to develop screening tools to help healthcare professionals to identify sepsis in their patients.
HOW TO SPOT SEPSIS IN CHILDREN
A child may have sepsis if he or she:
- Is breathing very fast
- Has a ‘fit’ or convulsion
- Looks mottled, bluish or pale
- Has a rash that does not fade when you press it
- Is very lethargic or difficult to wake
- Feels abnormally cold to touch
If you spot any of these signs, call 999 or go straight to A&E, and just ask, “could it be sepsis?”
A child under 5 may have sepsis if he or she:
- Is not feeding
- Is vomiting repeatedly
- Has not passed urine for 12 hours
If you spot any of these signs, call 111 or see your GP and just ask, “could it be sepsis?”
If your child has had sepsis and you are concerned that opportunities may have been missed in their treatment, our specialist sepsis negligence solicitors would be happy to talk it through with you.
We are proud to work closely with UK Sepsis Trust. More information about sepsis can be found on their website: https://sepsistrust.org